Your Sight Matters: Finding a Cure for Macular Degeneration
Age-related macular degeneration (AMD) is the most common cause of blindness in individuals over age 55 in developed nations and more than 10 million people in the United States have AMD, according to the Foundation Fighting Blindness.


in Arizona alone more than 2 million people were age 50 or older in 2010, according to the U.S. Census Bureau.
Age-related macular degeneration (AMD) is the most common cause of blindness in individuals over age 55 in developed nations and more than 10 million people in the United States have AMD, according to the Foundation Fighting Blindness.
AMD is particularly prevalent in the Southwest, with its large retired population; in Arizona alone more than 2 million people were age 50 or older in 2010, according to the U.S. Census Bureau.
The cause of AMD is unknown, but several risk factors — such as race and smoking — have been identified. Unfortunately, AMD cannot be prevented, and limited treatment options exist for those affected by the disease.
Two forms of AMD exist: “dry” and “wet.”
Dry AMD is the most common form. Beyond vitamin supplements, which show limited effectiveness in slowing vision loss, no treatment options are available.
Wet AMD involves the formation of abnormal blood vessels in the retina, a thin layer of tissue on the inside back wall of your eye. These new vessels often leak in the eye, further disturbing the tissues responsible for vision. Treatments can stop the growth of these blood vessels, which helps slow the progression of the disease in some patients, but this treatment plan requires repeated injections in the eye, which is painful, inconvenient and very expensive.
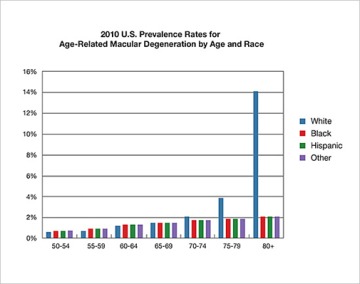
Age-related macular degeneration is much more widespread in the white population and a person’s natural coloring appears to protect people from developing the disease.
In short, better strategies to treat or prevent AMD are needed. In response, the McKay Laboratory at the University of Arizona has taken a new approach to stop the progression of AMD, based on the natural history of the disease.
It turns out the disease is much more widespread in the white population. Based on this information, researchers developed the hypothesis that pigmentation – a person’s natural coloring – appears to protect people from developing the disease. To test this hypothesis, the Mckay Lab and collaborators discovered a signaling pathway, a communication process that manages cell activity and actions, in the pigmentation system that protects the retina.
In addition, a molecule that can activate this pathway was discovered, suggesting this molecule could be targeted to treat or prevent AMD. The molecule, called Levodopa (L-Dopa), is a naturally occurring molecule made in all pigmented tissues, including the retinal pigment epithelium of the eye, where it has a role in maintaining a healthy macula, the part of the eye’s retina that provides the most high-acuity color vision.

The McKay Laboratory team includes (from left to right) Nicole R. Congrove, BS, Anna G. Figueroa, BS, Sara A. Sillik, Brian S. McKay, PhD, Rory Colvin-Morrison, BS and Mariel Piechowicz, BS (not pictured).
The combination medication carbidopa-leveodopa targets the L-dopa molecule and is the predominant treatment for movement disorders like Parkinson’s disease. L-Dopa has been the gold standard treatment for Parkinson’s since the mid-1960s, so its safety history is well-documented.
If taking a synthesized form of L-Dopa activates a signaling pathway in the pigmentation system that appears to protect from AMD, do people taking L-Dopa for Parkinson’s get AMD?
With data from medical records of more than 87 million individuals in the United States, researchers found that those prescribed L-Dopa were much less likely to develop AMD. In addition, the age of onset was delayed by more than eight years. L-dopa appears to prevent and delay AMD.
The lab continues to study AMD by investigating pigmentation from tissues involved in the disease. The McKay Lab is unique, in that it bridges the gap between basic laboratory sciences to clinical studies of the drugs discovered. Lab members work with community clinical collaborators Robert W. Snyder, MD, PhD, and Timothy Fagan, MD. Three clinical trials have been developed to test the effect of L-Dopa on AMD.

Age-related macular degeneration (AMD) is the most common cause of blindness in individuals over age 55 in developed nations and more than 10 million people in the United States have AMD.
These studies are investigating carbidopa-levodopa, a drug that is FDA approved. The ongoing clinical trials are recruiting subjects and are being conducted in Tucson, Arizona. The three studies are aimed at determining if carbidopa-levodopa:
- Stops the progression of the disease
- Reduces or prevents the need for injections in newly diagnosed wet AMD
- Stops or reduces the progression of geographic atrophy observed in dry AMD
Individuals who would like to participate should contact Snyder Eye Doc or McKay Lab.
In science and medicine, the gold standard in determining whether a drug works is proof from clinical trials such as these. Your participation may help your vision or the vision of someone you care about, but also will help to illuminate a path forward to prevent or treat this terrible and common blinding disease.
About the Author
Anna G. Figueroa received a Bachelor of Science degree from the University of Arizona in 2018, studying Neuroscience and Cognitive Science, Physiology, and Anthropology. Anna’s research in the McKay lab focuses on the role of extracellular vesicles and their potential role in cargo uptake between normal and diseased ocular tissue with the hope of further identifying communication pathways that cause Age-related Macular Degeneration (AMD).
About the Author
Brian S. McKay, PhD, is an associate professor in the Department of Ophthalmology and Vision Science at the Univeristy of Arizona College of Medicine – Tucson. Dr. McKay was trained in cell biology during his PhD studies at the Medical College of Wisconsin under Dr. Janice Burke and became interested in age-related macular degeneration (AMD). He trained in protein chemistry during his postdoctoral fellowship at The Scripps Research Institute before joining the faculty at Duke University in the department of Ophthalmology. Dr. McKay was recruited to the University of Arizona’s department of Ophthalmology and Vision Science, where he has been figuring out the link between race and AMD. The results of the novel research direction have brought his the McKay Lab to one of it's long-term goals, initiation of clinical trials to test whether AMD can prevented or treated.

