Addressing a Research Gap in Menopausal Asthma
A doctoral student is using the Infection and Inflammation as Drivers of Aging training program to investigate menopause-onset asthma.
Asthma is the leading chronic disease in children and is more common in boys than girls. Yet people can develop asthma at any stage of life, and as people age asthma becomes more common in women than men. The Centers for Disease Control and Prevention reports that nearly 10% of adult women have asthma compared to 6% of men.

Wil Pederson’s research is supported by the Infection and Inflammation as Drivers of Aging T32 Ruth L. Kirschstein Institutional National Research Service Award from the National Institute of Health.
In general terms, asthma is a condition where a person's airways become inflamed, narrow and swell, and produce extra mucus, which makes it difficult to breathe. In recent years, University of Arizona Health Sciences researchers have begun to investigate various subtypes of asthma.
“Asthma in adult males versus asthma in menopausal women versus asthma in children are radically different diseases with radically different drivers,” said Felicia Goodrum, PhD, professor of immunobiology in the UArizona College of Medicine – Tucson.
Just as each type of cancer is different and therefore not all treatments work on all cancers, asthma also presents differently and requires more precise treatments based on biomarkers and the type of inflammation that is occurring.
Wil Pederson, a fourth-year doctoral student in the Physiological Sciences Graduate Interdisciplinary Program, is exploring one of the least studied subtypes: asthma that begins in women at the onset of menopause.
“Collectively, we want research across the field to bring us molecular targets that can treat or prevent specific types of asthma. That makes the work that Wil is doing in this unique area very important," said Dr. Goodrum, a member of the BIO5 Institute.
“He identified a clinical need and was looking to go after a solution.”
-Julie Ledford, PhD
Pederson’s research, which mimics both asthma and menopause using animal models, is being supported through the Infection and Inflammation as Drivers of Aging program, funded by a National Institutes of Health training grant. The program is co-led by Dr. Goodrum and Janko Nikolich-Žugich, MD, PhD, head of the College of Medicine – Tucson’s Department of Immunobiology, through a UArizona Health Sciences strategic initiative to create defenses against disease.
Identifying a clinical need
For more than seven years, Pederson has worked in the laboratory of Julie Ledford, PhD, associate professor of cellular and molecular medicine at the College of Medicine – Tucson and a member of the BIO5 Institute. Dr. Ledford’s research focuses on asthma and respiratory infections, specifically how different proteins in the lungs affect or protect against asthma and respiratory infections.

The Infection and Inflammation as Drivers of Aging training program provides opportunities for faculty with expertise in infection, inflammation, immunology and age-related pathologies, including Julie Ledford, PhD, (left), to train students like Pederson (right), to develop strategies to enhance resilience and extend the portion of life spent in good health.
Pederson had attended several conferences and presentations with Dr. Ledford when he was struck by the realization that very little was known about what drives menopause-onset asthma.
“Every time I went to these talks, they would show a Venn diagram with the various subtypes,” Pederson recalled. “They all mentioned menopause-associated asthma, but they never went into detail about it. It was always in the back of my head, and I found it interesting.”
Pederson saw a clear clinical need for further investigation. Prior research suggests menopause-onset asthma tends to be more severe than allergic asthma and there are fewer treatment options, which leads to an increase in hospitalizations.
He approached Dr. Ledford about designing his doctoral project around menopause-onset asthma, specifically what causes it in the first place and how it can be treated.
“Those are two completely different problems to solve,” Dr. Ledford said. “So, when he first told me, I knew it was going to be a hard project. But I was excited for him. He identified a clinical need and was looking to go after a solution.”
Finding a way forward

Pederson has been working in Dr. Ledford’s lab for several years, during which time he has co-authored three papers with two more pending.
When Pederson began designing his own studies, he realized that one important piece was missing. While he could accurately model asthma in his studies, he was not aware of a model that could mimic what takes place at the molecular level during menopause.
Fortunately, Pederson was introduced to Heddwen L. Brooks, PhD, associate professor of physiology at the College of Medicine – Tucson. Dr. Brooks was using a new menopause model in her research on hypertension.
Pederson and his colleagues were able to combine the asthma and menopause models to develop a new one that will allow researchers to design more studies that begin to answer bigger questions about menopause-onset asthma. The research will be detailed in a paper that is awaiting publication.
“Now we can start to look at reasons why asthma is occurring during or after menopause,” Dr. Ledford said. “We can figure out what's driving this problem.”
Separating aging from menopause
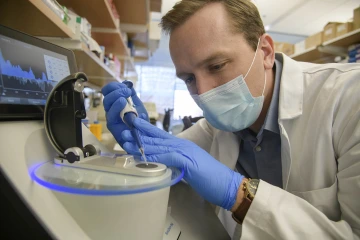
Pederson, a doctoral student in the Physiological Sciences Graduate Interdisciplinary Program, realized there was a missing piece needed to study menopause-onset asthma and was determined to find a model to fill that gap.
Pederson credits the Infection and Inflammation as Drivers of Aging training program for expanding his knowledge of aging, which was not an initial goal of his when he first approached Dr. Ledford with the idea of studying menopause-associated asthma.
“I’m able to bring knowledge about menopause and some of the hormonal changes, but it’s interesting to learn about the aging factors, too,” Pederson said.
He says one hurdle in the aging field is separating aging from menopause, as women experience menopause at different ages, with some in their 40s and others not for another decade or more. Thus, it is important to distinguish the physiological changes that occur at the onset of menopause from those that occur due to aging.
“That is one of the big challenges in menopause research,” Pederson said. “I think my project really offers some insight into that, because we can very quickly see the effects of just menopause on asthma, without the effects of aging.”
Our Experts
Contact
Blair Willis
520-626-2101
bmw23@arizona.edu

